Abstrak
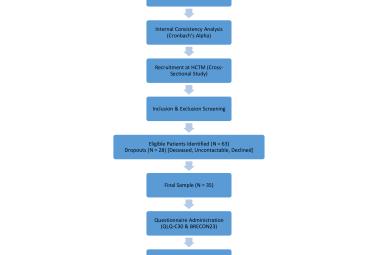
Polifarmasi psikotropik dalam kalangan para pesakit tua merupakan suatu permasalahan kerana mereka menghidapi pelbagai penyakit yang lain. Kajian ini menyiasat polifarmasi psikotropik dalam kalangan pesakit tua yang didiscaj daripada sebuah hospital pengajar di Malaysia dan menentukan faktor-faktor yang berkaitan dengannya. Laporan discaj pesakit berumur 65 tahun dan ke atas dari wad-wad psikiatri antara tahun 2010 sehingga tahun 2019 dikaji semula. Data sosiodemografik bagi tempoh kemasukan wad (‘Length of stay’, LOS), diagnosis psikiatrik dan lain-lain, serta preskripsi ubat psikotropik semasa discaj diambil daripada pangkalan data elektronik. Analisis ‘multiple logistic regression’ dilaksanakan dengan umur, jantina, bangsa, status perkahwinan, diagnosis psikiatrik utama, LOS, dan jumlah komorbiditi perubatan sebagai pembolehubah tidak bersandar, manakala polifarmasi (>2 ubat psikotropik) sebagai pembolehubah bersandar. Terdapat 354 discaj dalam tempoh ini. Purata usia ialah 72.4 tahun (SD-5.9 tahun) di mana 63.0% ialah wanita dan 39.8% ialah bangsa Melayu. Kebanyakannya telah berkahwin (84.2%). Kategori diagnosis psikiatrik yang paling utama ialah gangguan mood (54.5%). Sebanyak 76.8% discaj melibatkan satu atau lebih komorbiditi perubatan. Jumlah median ubat psikotropik ialah dua, dengan 38.1% terima tiga atau lebih ubat psikotropik. Dalam model ‘multiple regression’, didapati jantina perempuan, bangsa Melayu, dan berkahwin berkait rapat dengan polifarmasi psikotropik. Faktor-foktor sosiobudaya mungkin menyumbang kepada polifarmasi psikotropik dalam kalangan pesakit tua. Faktor-faktor begini perlu disiasat lebih lanjut untuk mengenalpasti peranan mereka.
Kata Kunci :
komorbiditi,
penyakit mental,
polifarmasi,
ubat psikotropik,
warga tua,