Incidence of Post Tuberculosis Chronic Obstructive Pulmonary Disease in a Tertiary Centre In Malaysia
Chronic Obstructive Pulmonary Disease
Abstract
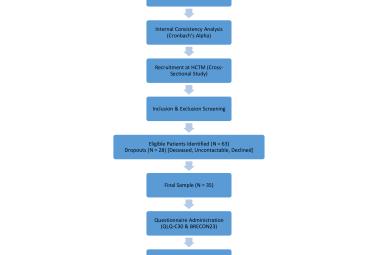
Pulmonary tuberculosis (PTB) and chronic obstructive pulmonary disease (COPD) are important causes of mortality and morbidity in Malaysia. The number of tuberculosis (TB) cases in Malaysia appears to be increasing and there were 500,000 Malaysians diagnosed with COPD in 2016. A substantial number of PTB patients go on to develop post tubular airway disease. Past infection with TB has been shown to contribute to the aetiology of COPD. We conducted a one year cross-sectional study in outpatient setting involving adult subjects in Universiti Kebangsaan Malaysia Medical Centre (UKMMC) with a history of pulmonary tuberculosis three years prior to the study. We excluded subjects with bronchial asthma, COPD, interstitial lung disease and bronchiectasis. Airflow obstruction was defined as FEV1: FVC ratio <0.70. The COPD Assessment Test (CAT) questionnaire was used. Eighty-two subjects were recruited with a median age of 52.5 years (IQR 36-62). Male predominance (56.1%) with 29 (35.4%) smokers. Eighteen (22%) subjects had airflow obstruction. Six (33%) out of these subjects were smokers. Fourteen(17%) had restrictive pattern and 50 (61%) had normal spirometry results. Five subjects (22.22%) had mild obstruction, 7 (44.44%) moderate obstruction, and 6 (33.33%) had severe obstruction. There was a positive correlation between chest X-ray abnormalities and age with airflow obstruction (P<0.05). Abnormal spirometry pattern was found in 39% of subjects. Post TB-COPD incidence was 22% in those who completed TB treatment. There appeared to be an association between abnormal chest radiograph findings with airflow obstruction in subjects with history of PTB.
Keywords :
airway obstruction,
chronic obstructive pulmonary disease,
pulmonary tuberculosis,
Abstrak
Tuberkulosis (TB) paru-paru dan penyakit “Chronic Obstructive Pulmonary Disease” (COPD) adalah punca utama kematian dan morbiditi di Malaysia. Di Malaysia, jumlah kes TB semakin meningkat dan terdapat 500,000 rakyat Malaysia yang didiagnosa dengan COPD pada tahun 2016. Sejumlah besar pesakit TB mendapat “COPD” pada jangka panjang. Jangkitan TB yang lepas telah terbukti menyumbang kepada etiologi COPD. Kami menjalankan kajian keratan rentas selama satu tahun yang melibatkan pesakit dewasa di klinik pesakit luar di Pusat Perubatan Universiti Kebangsaan Malaysia (UKMMC) yang mempunyai sejarah TB paru-paru 3 tahun sebelum kajian. Pesakit yang dikecualikan adalah pesakit asma, COPD, penyakit paru-paru interstitial dan bronchiectasis. Obstruksi aliran udara ditakrifkan sebagai nisbah FEV1: FVC <0.70. Soal Selidik Ujian COPD (CAT) telah digunakan. Lapan puluh dua pesakit telah direkrut dengan umur median 52.5 tahun (IQR 36-62). Pesakit lelaki seramai 56.1% dengan 29 (35.4%) perokok. Lapan belas (22%) mempunyai masalah aliran udara di mana enam (33%) dari subjek ini adalah perokok. Empat belas (17%) mempunyai “restrictive pattern” dan 50 (61%) mempunyai spirometri normal. Lima subjek (22.22%) mempunyai “mild obstruction”, 7 (44.44%) “moderate obstruction”, dan 6 (33.33%) mempunyai “severe obstruction”. Terdapat korelasi positif antara keabnormalan sinar-x dada dan umur dengan obstruksi aliran udara (P<0.05). Corak spirometri yang tidak normal didapati dalam 39% subjek. Post TB-COPD insiden adalah 22% pada mereka yang tamat rawatan TB. Terdapat kaitan antara penemuan radiografi dada yang tidak normal dengan halangan aliran udara dalam subjek dengan sejarah PTB.
Kata Kunci :
Jangkitan Tuberkulosis Paru-Paru,
Obstruksi aliran udara,
Penyakit Paru-Paru Obstruktif Kronik,
Correspondance Address
Mohamed Faisal Abdul Hamid. Respiratory Unit, Department of Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Jalan Yaacob Latif, Bandar Tun Razak, 56000 Cheras, Kuala Lumpur, Malaysia. Tel: +603-91456018 Email: faisal.hamid@ppukm.ukm.edu.my